Live. Magazine
“Even without a microscope, you can sometimes see with your naked eye that the mini-hearts are beating,” says Makoto Hara, a group leader in the Cardiovascular Discovery unit at Novartis Biomedical Research.
“When I remember the first morning that I saw this working, I was so excited that I took the video home to show it to my daughter – and the whole team knew that we could finally begin answering the research questions we had been asking for so many years,” Hara says.
The exciting sight of these pumping mini-hearts has been the fruit of a years-long collaborative effort between different research teams, ranging from biologists and drug hunters to data and engineering experts.
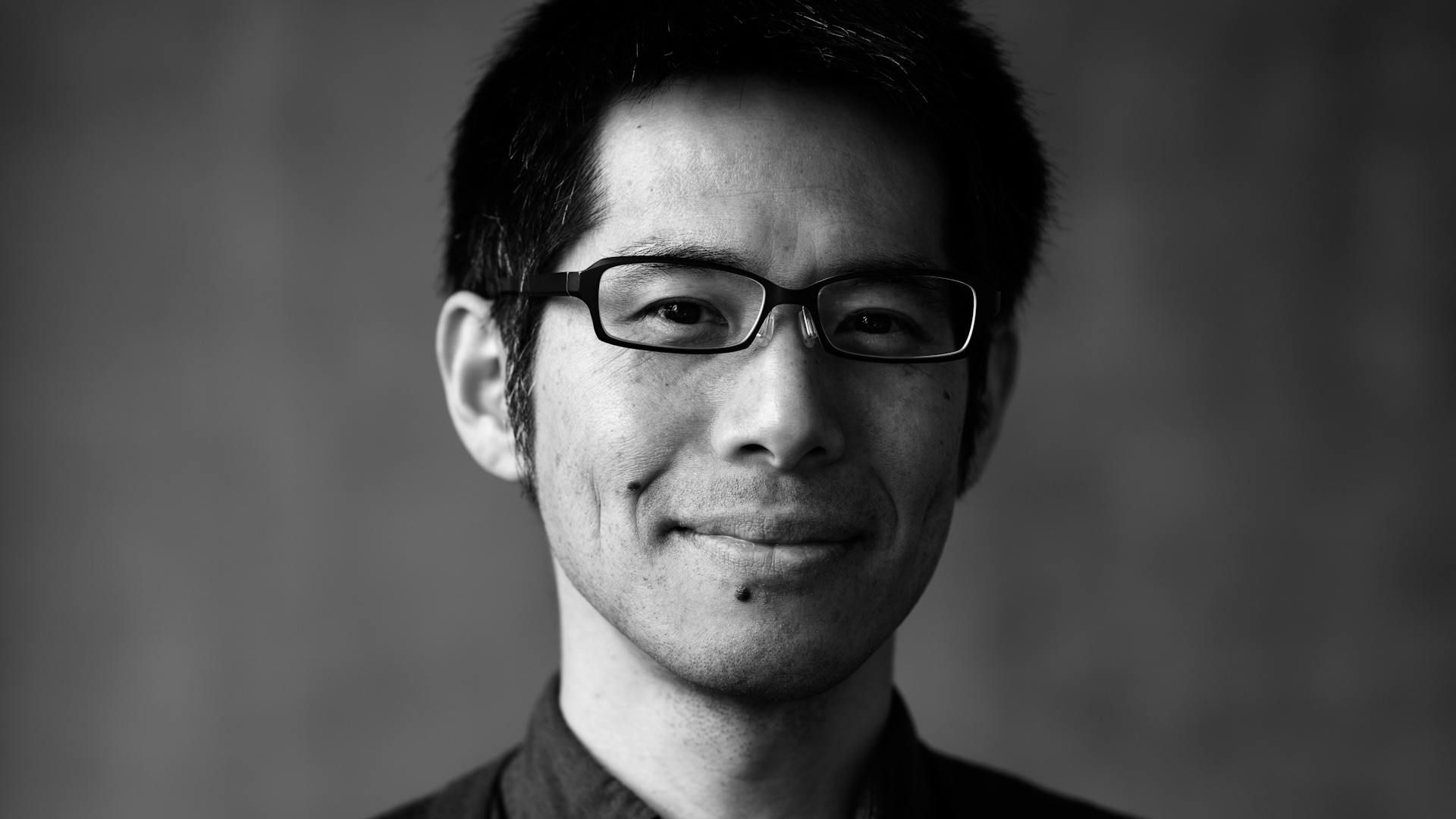
Makoto Hara:
Never give up.
The whole effort was kick-started in the mid-2010s, when the team began working on a drug target that had been shown by academic researchers to play a role in how heart muscles relax. Finding a molecule against this target was considered ideal to develop a heart failure treatment in which the heart struggles to pump enough blood through the body.
But Hara and the team faced major challenges. The target was out of reach using conventional research methods. Classic compound testing, which uses 2D layers of animal or human cells, lacked essential elements which Hara needed to reach.
From 2D to 3D
Hara’s group initially wanted to understand how the heart relaxes under the influence of a compound. For this, their model would need to be 3D and behave like a heart to generate the needed insights.
While Hara and his team tried for several years to get as much as possible out of conventional methods, their efforts received a major boost when they heard from their Novartis colleague Brian Clark about the possibility of upgrading their 2D model and creating 3D miniature hearts for drug testing.
The posts on the testing plates move with the beat of the mini-hearts, allowing researchers to quantify the force they produce.
“In 2D tests, we could measure how quickly the cells were beating, but we couldn’t quantify the strength, or force, of the beats, or how fast the cells relaxed,” says Hara. “And this was the information we really needed and that we wanted to get with the help of the 3D model.”
To create the updated model was far from easy. It took a multi-year effort from various teams. Besides creating the mini-hearts with the help of induced pluripotent stem cell (iPSC) technology, researchers worked on special plates to allow the mini-hearts to beat like real ones. They also created a video system that captures the beating hearts and a bespoke data analysis method using AI.
Hara’s team, including Swetha Siva and Lucas Goguen, worked on the cell culture side of the platform. Siva, working with team member Joe Wamstad, took iPSCs from human skin cells and coaxed them into heart muscle cells called cardiomyocytes by applying a cocktail of agents. These cardiomyocytes formed the basis of the mini-hearts.
But this was only the first step on the way to developing the platform. To allow the mini-hearts to beat like real hearts, the team collaborated closely with system engineers who designed specialized testing plates that had two small flexible posts in each well.
Each mini-heart could then be tethered around those posts. When the mini-heart would beat, the posts would move as well. This provided a way to quantify the force produced during each mini-heart beat – answering one of Hara’s key questions.


An important part in setting up the system ...
... was constructing the plates that hold the mini-hearts.
Video …
But it took several iterations and continuous development to make this work well. For example, team members Vipender Singh, Savannah Moore and Alex Clark found an additive that strengthened the mini-hearts, helping them to last for months and be reused for multiple different screening experiments. This also allowed expansion of the platform to test multiple types of drugs and enabled target validation efforts.
The innovation motor did not come to a halt during the coronavirus pandemic either. When a key ingredient for making mini-hearts became unavailable due to pandemic-related supply chain issues, Singh also enabled an alternative method. Singh and Clark then collaborated with the engineering team to co-develop a new type of the mini-hearts plate that worked better with the new method, which is now incorporated in our latest system by other team members.
In addition, the team also had to design and install a camera system to capture the movements, as well as develop a data analysis system to interpret the results.
“In the early days, we built the platform from scratch, with components literally taped together, and the initial prototype took a video of one mini-heart at a time, which meant that an experiment for a single test compound could take a full afternoon,” says Hara’s colleague Gordon Turner.

Gordon Turner:
The magic of data.
A second version of this set-up used eight cameras, each attached to a separate dedicated computer, which made it possible to run eight experiments in parallel.
“But over the past several years, this broad-based collaboration has made it possible to scale up the platform to 96 experiments at a time and to create a data analysis tool so that the biologists can have the results within a few minutes,” Turner says.
But innovation won’t stop here: “We are also testing the latest improvements, which are designed to scale up the platform to 384 experiments at a time,” Turner adds.
Machine learning
Turner, who today heads the data science group within the Cardiovascular Metabolism Research unit, also helped develop a data analysis tool to rapidly process the data coming from the mini-heart videos.
To make the program easily accessible to all researchers, Turner’s team created a webpage where biologists can enter their data and receive the analysis with just a few mouse clicks.
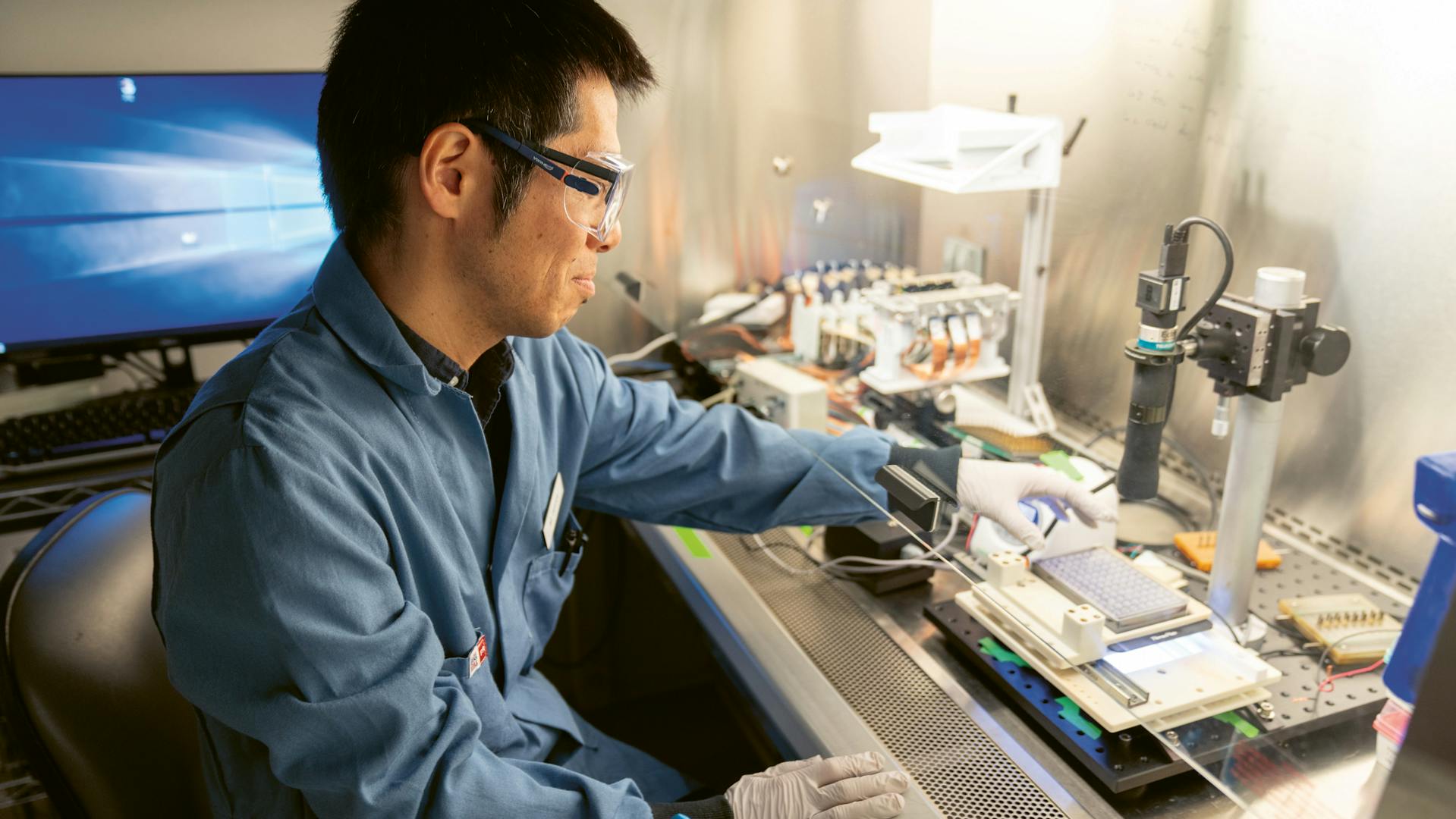
Makoto Hara sets up the camera system that will film the mini-hearts. It took him and his team several years to achieve this breakthrough.
Cardiomyocytes used in the experiments contract and relax exactly like they would in a real heart.
“The web app may seem minor, but inputting the data was a big impediment to the biologists using the system,” says Turner. “Now the analysis takes just a few minutes and that’s been really transformational for everyone.”
Recently, the team has also added machine learning – the ability of computers to efficiently analyze images and match patterns – to help make the process even faster.
“Early on, we had a process where we would ask the user to put a box around each post manually,” explains Turner. “You can imagine that works okay for one or two videos, but now we’re doing 96 videos at a time and we needed a faster solution.”
To address this issue, Turner’s colleague Michael Chien-Cheng Shih from Novartis in San Diego developed a computational model that he trained to recognize and track the posts automatically.
“As our colleagues create new methods to collect increasingly complex data, analyzing those results can become a roadblock,” says Shih. “My group’s role is to provide tools that can be quickly adapted for new purposes and to give our colleagues the confidence that the data analysis isn’t going to be a limiting factor as they scale up to larger datasets.”


To make the mini-hearts beat, the team is using electrodes
The experiment is continually monitored.
Collaboration
The continual improvement of the mini-heart platform has helped Hara’s group drive their research project forward, allowing them to find a number of potentially interesting molecules, which are now being optimized into potential lead candidates.
“The results that we’ve seen with the mini-heart platform have given us confidence that this could one day lead to a good medicine for heart failure patients,” Hara says. “That’s the motivation behind the work we’re doing.”
Collaboration, he says, has been crucial for this. “In addition to our own work in heart failure, the success of the mini-heart platform also owes much to the efforts and dedication of our collaborators across the company,” says Hara. “Each step of the development required customized solutions and it has taken many years to get the platform ready for use in drug screening, but we’re happy to say it’s finally ready for broader use.”
Multipurpose platform
The success of the platform has also attracted the attention of other cardiovascular research groups in the company. It has since been expanded to more projects, particularly profiling different genetic targets in other cardiovascular diseases such as hypertension or arrhythmias.
“When we identify new genes to target through clinical trial data, we use the platform to mimic the associated human diseases and learn more about the effects of those genes,” says Turner. “One of the huge advantages of the platform is that the organoids are originally derived from human skin cells, so we can see what’s happening in a human context, as opposed to using animal models, which are often not translatable.”
Organoids such as mini-hearts have become possible with the development of induced pluripotent stem cell (iPSC) technology.
The platform’s data analysis tool has also proven useful for experiments beyond the heart muscle force calculations that were needed for Hara’s research project.
In cardiovascular research, there are other properties that change over time and are essential for healthy heart functioning. These include the influx of calcium molecules or altered voltage (as measured in electrocardiograms, or ECGs). The platform’s data analysis tools are now also providing an improved method for these experiments. The platform also works well for toxicity studies.
In fact, the platform has been receiving far more requests than the group has capacity to provide. “The idea began with the target that I was working on, but we’re applying the platform and the data tool to more and more different cases now too,” says Hara. “Along with our collaborators, we’ve invested many years into developing this platform and now we’re seeing dividends across the cardiovascular division and maybe, in the future, in other disease areas too.”







