Live. Magazine

Travels in medicine
Joysticks and neuroscience.
New paths into the brain
Just a few years ago, paralysis or speech loss were a common consequence of strokes. While the treatment of this acute condition remains extremely challenging, there are rays of hope. Marios Psychogios, Head of Neuroradiology at University Hospital Basel and professor, makes a significant contribution to improving the quality of life of stroke patients with his work and research projects.
Text by Michael Mildner, photos by Adriano A. Biondo.
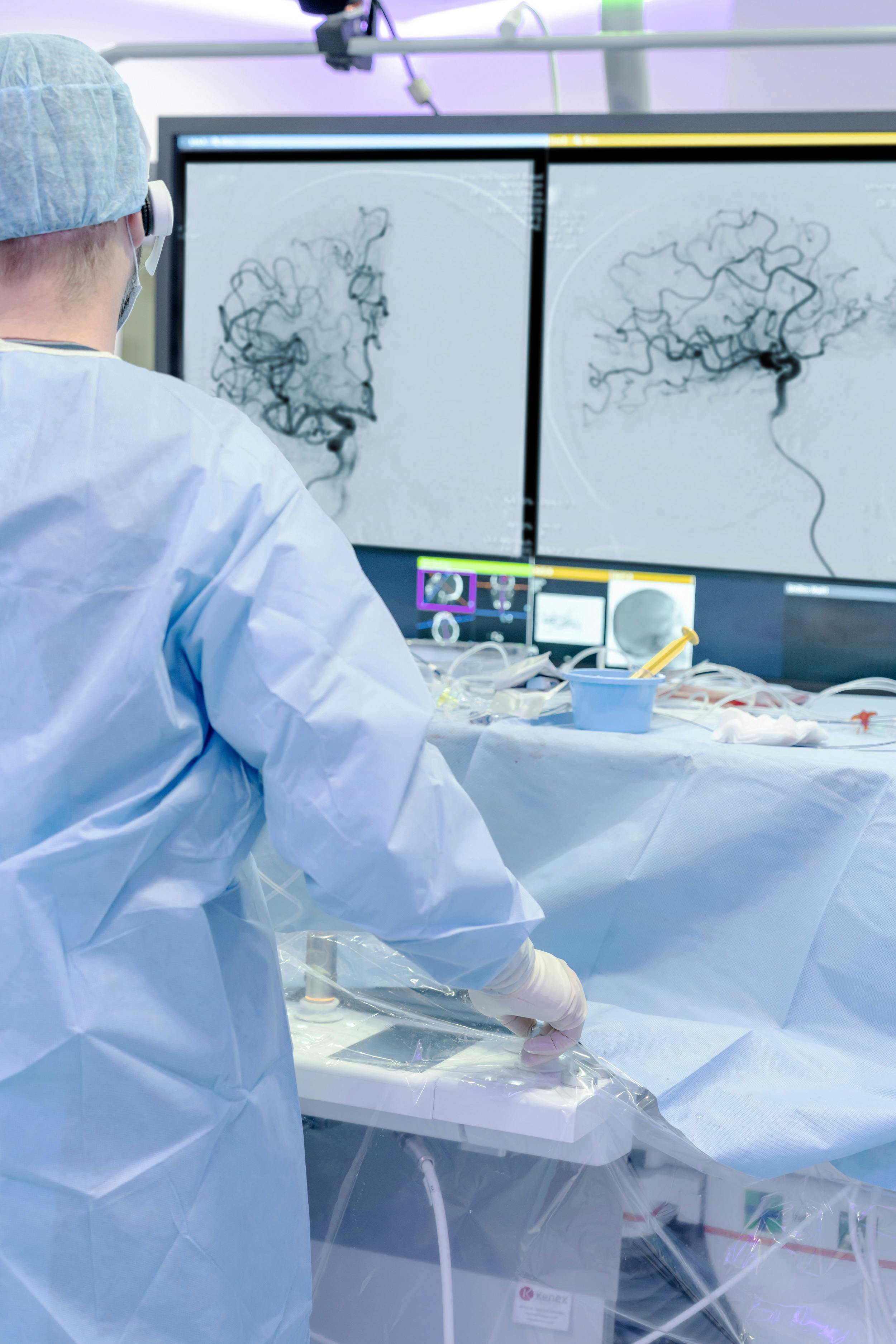
The interview was scheduled for 10:00 a.m. As the clock ticks around, it becomes clear that Marios Psychogios will not be able to join us on time. We were warned in advance that something might come up. Instead of being interviewed, the doctor now stands in the operating theater and is doing everything in his power to treat a stroke patient who has just been rushed to the University Hospital Basel. We are able to follow the procedure on a monitor in Marios Psychogios’ office.
We see a black spot on the screen. It shows the clot in the patient’s head. The entire area behind it is practically colorless and therefore no longer supplied with blood. The longer this lasts, the greater the irreversible damage caused by this serious stroke.
Psychogios stands in the operating theater and is doing everything in his power to treat a stroke patient who has just been rushed to the University Hospital Basel.
About an hour later, Psychogios exits the operating theater relaxed and in a good mood. The procedure has been successful, the patient’s brain is once again fully supplied with blood, and there is a good chance that the patient will be able to live a normal life again. But successes like this are by no means taken for granted. Severe paralysis, speech impairment or even a complete loss of speech are some of the potential risks of this condition, which affects 16,000 people every year in Switzerland and is the third leading cause of death.
Following the procedure on a monitor.

Better chances for patients
“Over the past 15 years, we have made great strides in treating stroke patients like this,” says Psychogios. One important lesson that the doctor learned from his many years of working at German and Swiss hospitals was the importance of time. “It’s not just the opening of the vessels that is important, but also the time it takes. If you open the vessel after five or ten hours, the results are worse than if you open it after ten minutes,” he explains.
What sounds logical today was not something that could be taken for granted in the 1980s. Back then, the advice was to only take a computed tomography after one to two weeks – with corresponding negative consequences for the health of patients. “Ideally, we can now remove the blood clot within 30 minutes of the patient being admitted to hospital,” says Psychogios with visible satisfaction. Despite these successes, however, the doctor is convinced that the path to improved patient treatment is far from over.
This also applies to the path that Psychogios himself chose as a young medical student when he moved from his native Crete to Germany in 2005 on an Erasmus scholarship. “I had always done a lot of exercise and wanted to become an orthopedic surgeon. However, during my internship in the neurology department, I was allowed to accompany a patient with a recent cerebral hemorrhage to the examination room. I watched the whole treatment process, and it fascinated me so much that I stayed in the cooler surroundings of the north to start further training in radiology and neuroradiology,” he recalls.
The motivation to start working on research projects came from his supervisor at the hospital in Goettingen. As a reward for publishing a paper, he gave the junior doctors a few days off each time. “As I have always had a strong affinity for the sea and diving, this was reason enough for me to start my first projects. I never imagined back then that my research would eventually lead me to Basel and a professorship at the university,” says Psychogios.
Plumber, watchmaker, and doctor
When asked what exactly a neuroradiologist does, Psychogios first compares his work with a plumber who opens and closes water lines, and then mentions the need for finesse as is required by watchmakers. This modesty is typical of the down-to-earth doctor who, even decades later, still pursues his profession with the same passion as he did at the beginning. The diagnostic aspect of his work and the combination of imaging diagnosis and interventional therapy is what makes his profession so fascinating.
According to the dictionary, neuroradiology is a branch of radiotherapy that allows for the diagnosis and treatment of neurological diseases. Magnetic resonance tomography, computed tomography, but also invasive procedures – known in the field as angiographies – are used to make a diagnosis. A contrast medium is injected into the blood vessels, which is followed by an imaging procedure using X-rays, computed tomography, or magnetic resonance imaging. The Department of Neuroradiology, headed by Psychogios at the University Hospital Basel, is primarily concerned with this method of examining the brain.
Marios Psychogios likes to play video games to train his dexterity. Working with minute tools has always been one of his biggest passions.

However, it takes a lot of patience and a strong will to do this job, as Psychogios knows all too well from his own experience: “After medical school, you first have to become a specialist in radiology, then you have to train in diagnostic neuroradiology, and if you’re still interested, invasive neuroradiology follows. At the end, you are a kind of potpourri of different skills and roles.”
In day-to-day hospital environment, the work of a neuroradiologist is divided into diagnostics and intervention. As a radiologist, Psychogios primarily looks at scans from computed tomography (CT) or magnetic resonance imaging (MRI) in order to make diagnoses. When it comes to intervention, he takes on a role similar to that of a neurosurgeon. Enormous progress has been made in this area in particular in recent years.
In the past, all vascular pathologies and vascular malformations were operated on in open surgery. The procedure is now minimally invasive, with surgeons making their way through the inguinal artery or wrist artery with a small tube to the brain, where the treatment takes place.
This procedure uses two X-ray machines for imaging. Psychogios is often asked whether the catheter has a camera during the procedure: “The monitor shows us working with our hands on wires and catheters. But we don’t have a camera. We use the radiation from these two X-ray machines, which show me on the monitor how the wires and the catheter are manipulated by subtle movements of my hands.”
The long path into the brain
Without the discovery of X-rays around 100 years ago by Wilhelm Conrad Roentgen, none of this would be possible. This also marked the beginning of radiology. The next important step in angiography was the work of researcher and doctor Sven-Ivar Seldinger, who developed the method for penetrating blood vessels and inserting a small catheter.
Even watchmakers would be impressed by the size of the instruments used by Psychogios and his team.

The most important innovation, however, is related to The Beatles. The band was so successful that their record label EMI was able to invest in other areas as well. One of those investments was in the company established by Sir Godfrey Hounsfield, a Briton who designed the first CT scanner. Finally, it was possible to create an image of a brain tumor in a patient where a diagnosis had proven difficult up to that point. Before, there was no way of looking into the intact brain or the skull. Back then, it took seven minutes to record and another ten minutes to develop the films – today, a CT scan of the skull only takes three seconds.
His instruments on the operating table.

Basel also played a role in this historical development. In 1974, the University Cantonal Hospital in Basel, as it was then known, bought the first CT scanner in mainland Europe. The innovative hospital used the device to diagnose brain tumors or cerebral hemorrhages and was thus able to detect or rule out hemorrhages accordingly. This was an essential point in the treatment of strokes. If a cerebral hemorrhage could be ruled out, treatment with a very strong blood thinner was possible. Unfortunately, this drug only works in the first few hours after a stroke – and even then only in 20 to 30 percent of cases.
Investigative spirit and finesse
The theoretical and practical findings of Psychogios have made an important contribution to further advances in the treatment of stroke patients. As a researcher who constantly questions the status quo and as a practicing physician who applies and refines his finesse directly in the brains of hundreds of patients every year, he is always looking for better solutions and new ways to reopen the closed vessels in the brain, giving patients a better chance of recovery and a better quality of life.
Details of the SAVE technology developed by Psychogios and his team were published for the first time in 2017. The innovative procedure is now used by doctors all over the world. The use of catheters and stents for the treatment of vascular occlusions is nothing new; these instruments are also used in the SAVE procedure. What is new, however, is the way and the order in which they are used. When to start aspirating and where to place the stent retriever, for example, both have a major impact on the result.
Psychogios describes the new approach: “We place the stent retriever, which looks like a small round wire fence, further away from the clot than was previously the case. As a result, it now only covers about a third of the clot. We then proceed with the catheter through the round opening on the mesh to the top edge of the clot and try to pinch it between the catheter and mesh.” Ideally, this results in a kind of sandwich – the technical term is “wedge position.” During withdrawal, the stent retriever, catheter and of course the clot are all removed together from the vessel, leaving it open again. With this technique, Psychogios and his team are now able to open more than 95 percent of vessels.
“... And then, all of a sudden, the patient can speak again. It’s difficult to put into words, it’s like a small miracle every time. …”
Marios Psychogios

No matter how many times he sees it, this is always an unforgettable experience for the doctor: “As soon as the clot is removed, blood circulation is also restored. Blood flows back to the affected area of the brain, and the clock is stopped on this stroke. And then, all of a sudden, the patient can speak again. It’s difficult to put into words, it’s like a small miracle every time. The patient is suddenly able to speak again or lift their arm…”
Time as deciding factor
As not only the removal of vascular occlusions, but also the time until treatment has a decisive influence on the chances of recovery of the patient, Psychogios also addresses this issue. During his time at the hospital in Goettingen, he and his team developed one-stop management, an optimized and time-saving treatment process. He briefly explains this as follows: “If you are very fast in treating a stroke, it normally takes at least an hour. By combining CT diagnosis and angio/imaging with therapy on the same device and in the same room, we were able to save half an hour – a time that improves treatment outcomes by around 10 percent.”
Combining CT diagnosis and angio/imaging with therapy on the same device and in the same room.

If you compare the progress made in recent decades with a Formula One race, the car with the fully treated stroke patient would already be at the finish line today – in the 1980s, the car would still be in the pits changing tires and refueling.
Despite all the successes, Psychogios often deals with serious cases and the struggle for life and death in his daily work in the hospital, a situation that can be stressful. “As a doctor in this field, I had to learn to be resilient. Sometimes, despite all efforts, the treatment does not succeed. Then you say to yourself: I’ve tried everything I can, but it just doesn’t work. From a human perspective, this is almost impossible to deal with – instead, you have to look at it from a technical perspective. Then there are the positive experiences, of course.”
The doctor tells us a story from a few weeks ago, where a 40-year-old patient with many risk factors was treated for a severe narrowing of the cerebral artery. After the stent was inserted, the artery was reopened, and everything seemed fine.
“But sometimes the stents close again… I was on duty,” Psychogios remembers, “and got a call at 2:00 a.m. the same night asking what to do. We tried unsuccessfully for three hours to reopen the stent, until we were finally able to reopen the vessel using different materials and other medication. These are the moments that you live for as a doctor.”
Deeper into the brain
A practice at the University Hospital Basel with more than 400 procedures a year, day and night shifts, a professorship at the university and interviews to boot – you would think this would be enough for a fulfilling professional life. But the 43-year-old doctor – who looks much younger – simply smiles and reports enthusiastically about a new medical study that he describes as a “hobby” in addition to his clinical work and his professorship at the University of Basel.
This study is called DISTAL and was started in 2021. The key question that Psychogios and his team want to answer with this study is: Can the disease burden of a stroke patient in the case of occlusion of a medium-sized cerebral artery be reduced with endovascular therapy, for example, by using stent retrievers or catheters?
While this form of therapy is already used as the standard procedure for occlusion of a large cerebral artery in the anterior areas of the brain, its benefit for medium or small-sized cerebral artery occlusions has not yet been conclusively researched. These types of occlusions are distal, i.e., further away from the heart and deeper in the brain. They occur in around a fifth of all serious cases.
“Until now, drug therapies have been used to treat these conditions,” explains the doctor and study leader, “but with DISTAL, we are investigating whether the combination of endovascular therapy and drugs leads to a reduction in the disability and dependency of stroke sufferers. The data from this study could provide the basis for treatment guidelines that have been missing up to now. This would be another valuable step in improving patients’ quality of life.”
The study was mainly funded by the Swiss National Science Foundation and the Bangerter Foundation for Swiss Patients. By acquiring additional funding from companies, the project was then expanded to the whole of Europe. This increases the chance of reaching the planned number of 500 patients within the next one to two years. If restricted to Switzerland, this would only have been possible after at least 10 years – if at all.
Organizationally, the study is managed by Luzia Balmer, who works closely with Psychogios. “We want to open around 50 study centers in Switzerland and Europe to enroll these 500 patients. 12 sites are currently participating in the study, with a total of 60 patients. All the major Swiss hospitals are already taking part, which was very important to us. There is a lot of interest and new centers are constantly being added in Europe, so we are very confident that we will have reached our targets by 2025 at the latest.”

Short chat after the procedure.
What the future holds
Robotics is probably one of the most exciting topics in the field of medical development at the moment. Like many other doctors, Psychogios believed for a long time that this would never be relevant to him. This attitude only changed when he heard about Vitor Pereira’s examinations using robots, which were first carried out in Toronto in 2019.
“It’s fascinating to see what Pereira has done over the past two or three years and how things will develop in future. Relatively soon, I think we will no longer carry out the procedure with our hands, but instead with the help of a robot like this,” says Psychogios.
The robot used in Toronto can move and rotate catheters and is controlled via a console that allows doctors to view images and operate joysticks. While the doctor still guides the catheter by hand, a robot works between them and the patient.
The question arises as to why this new constellation is needed in the first place. Improved protection against radiation for the treating doctor is certainly a valid point, as is the option of performing the operation sitting down – today’s treatments often last several hours and are often carried out standing. But for Psychogios, other aspects are crucial: “Emergency treatment is our business. If a patient has to be treated at night, we can’t tell them to drop by the office tomorrow and we’ll take a look, like in non-emergency cases, for example.
Our idea is to find a partner on the other side of the world who is currently working the day shift and can take care of the treatment for us. Conversely, we then deal with emergencies that arise during their night shift. This would allow us to form a global network and further improve the quality of treatment for patients.”
These new technical options could lead to several robot control centers being set up in Basel that are then operated from here in other countries. In any case, Psychogios already used the COVID lockdown to further develop his skills at the controller, and he is already in contact with the new professor of robotics in Basel. “Everyone has to have a hobby,” as he says.
Prospects for patients
The time it takes to remove the clot in the event of a stroke is crucial, as millions of neurons are irretrievably lost every second. As a result, the chances of a patient who has suffered a stroke on a remote mountain, for example, are still extremely poor.
Marios Psychogios with his Team at University Hospital Basel.

Psychogios and his team are also working on this problem. “The solution would be a drug that is given immediately after a stroke and freezes everything in the patient’s head. We call this neuroprotection. There have been countless studies on this, and we were involved in one of them two years ago. Although there was little effect of this drug in the overall population, there was a subgroup of patients where a very strong effect was seen.”
For this reason, the team in Basel is now participating in a follow-up study. But Marios Psychogios is already thinking further ahead. “Such a drug would have a lot of potential,” he says, “and you can, of course, imagine its future possibilities. There would then be syringes filled with the drug on the International Space Station or somewhere in the Alps. Patients then have time to be flown to hospital without their condition getting worse. As you can see, there are still many stages and paths on the journey into the brain that have not yet been explored.”






