Live. Magazine
Joerg Eder, a scientist at the Novartis Institutes for BioMedical Research (NIBR), still vividly remembers the afternoon call from his colleague Mark Keating asking him – out of the blue – whether the project he was working on was still making sense.
This was around 2009. Some four years earlier Eder and his team had launched the project together with Keating’s ophthalmology unit. It came on the heels of a scientific breakthrough that unveiled the underlying genetic mechanism of an eye disease that blurs vision and can lead to blindness.
The findings, which had been published in three separate papers in Science in 2005 and focused on the so-called alternative complement pathway of the immune system, had not only prompted Novartis to focus on this area. A slew of big and small biotech firms had entered the field too, triggering fierce industry competition.
“We had been on a pretty successful trajectory until then, when Mark asked me: “Do you think this will be successful?” Eder, an experienced drug discoverer who had started his scientific career at Sandoz, recalled the moment he had been confronted by his colleague. He understood where Keating’s question came from. Novartis was simultaneously working on several different approaches to tackle the disease along this specific pathway. Besides the classical chemical compounds Eder’s team was helping to develop, the company was also pursuing projects involving biopharmaceuticals.
Keating needed guidance on where to invest. “I knew there can be no guarantee for success when it comes to drug discovery,” Eder said. “But I was fully convinced that our approach was scientifically sound, so my answer was a clear: Yes, we can do it.”
Keating, a geneticist, followed Eder’s advice. But despite his backing, the team hit a dead end just a few years later, when Novartis decided to discard the small-molecule program and instead invest in the biologics venture and test these molecules in clinical trials. “This was a heavy blow to all of us invested in this project,” Eder said. “But it was clear that Novartis had to make a decision, since the company could not test all compounds in the clinic. It was a strategic move we had to accept.”
Hitting a wall …
By 2011, the team had a valid compound, yet it lacked a clinical strategy, as the door to test the experimental drug in opthalmology was shut. Worse, the Protease Platform headed by Eder with its more than 80 scientists, which had been one of the key drivers of the project, was also disbanded. In a nutshell, the project was destined to sink into oblivion.
But Eder, who moved to a new group in the immunology disease area, did not give up so easily. “I was really convinced that we did everything right in terms of the science and that the compounds we had developed up to that point could serve patient needs,” Eder said. “So, we continued and tried to find a new indication to work on.”
Embarking on developing a new clinical strategy, Eder received support from scientists such as Dick Harris, Anna Schubart and Stefanie Flohr, among many others, who were ready to help pivot the project from eye care to a new, yet-to-be-defined disease area.
The power of stamina
While this change of direction required stamina, endurance had been the name of the game from the first day of the project.
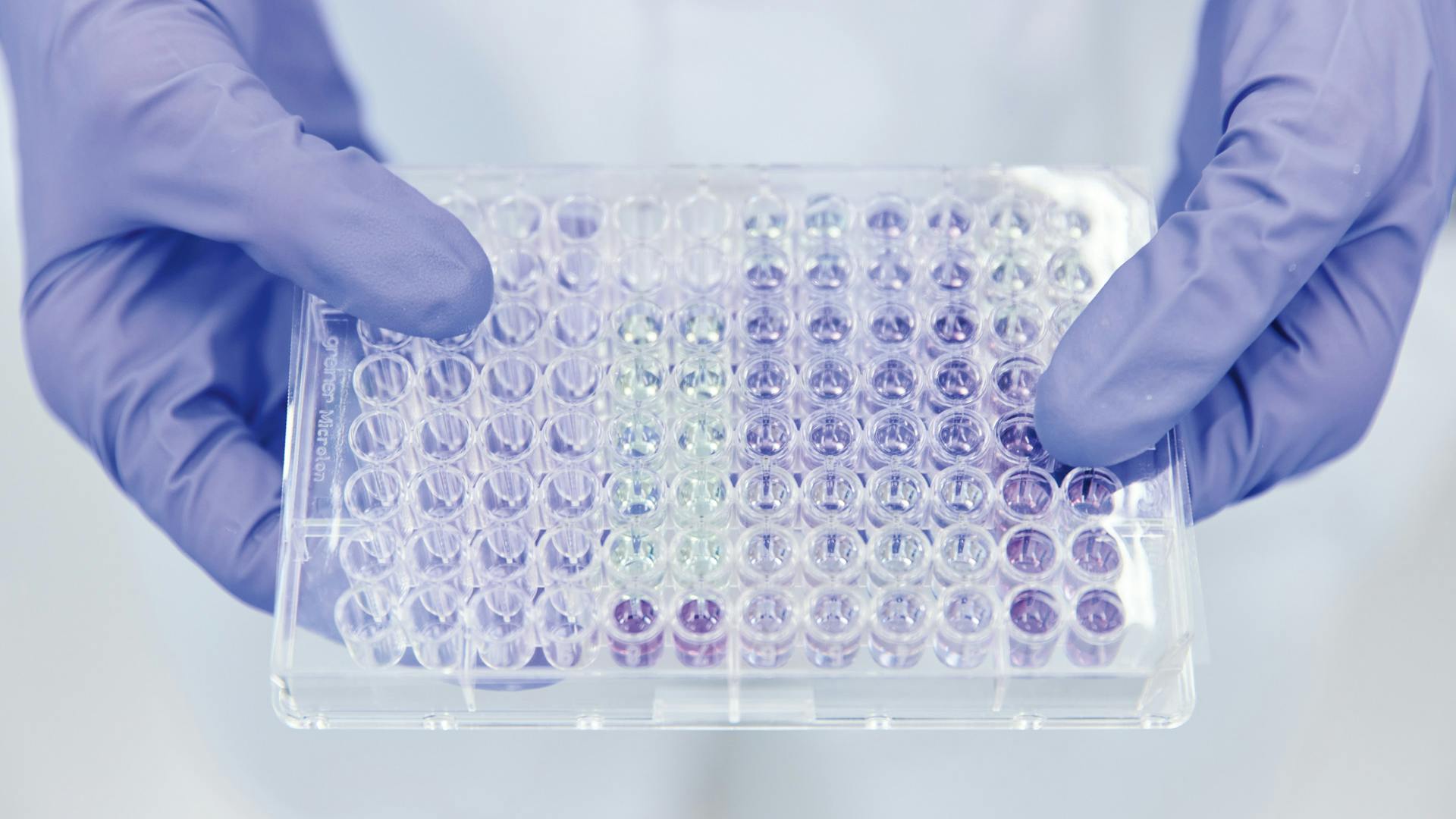
Soon after the publication in Science in 2005, the team had already run a series of high-throughput tests to find potential lead compounds that could serve as a starting point for the two targets that were identified in the research papers. But, to the team’s disappointment, they could hardly find anything with noticeable activity. “We made several high-throughput screenings with the more than 1 million compounds from our library. But all we found were a few compounds that showed limited activity,” Eder said.
To some extent, this was not a surprise. The targets that were identified in Science were difficult ones – to say the least. The proteins in question, Factor D and Factor B, which are part of the so-called alternative complement pathway, a sort of first defense line of the immune system, lack a clearly discernible active site, where scientists usually intervene by finding pockets to neutralize a disease-triggering cascade in the body.
“The fact that the two proteins we wanted to target didn’t have a fully formed active site made it very difficult from the start,” Eder said. “And the fact that we found almost nothing in our compound library made it almost impossible to continue.” Eder’s team, however, did not give in and came up with an ingenious idea. Instead of building on the single molecule that showed the strongest activity, the team picked elements from several molecular entities that showed some activity and started to build the compound in this way, taking a few atoms from each molecule that exhibited some binding capacity.
Jörg Eder
As a drug discoverer, it’s been my dream to help create a drug that makes it to the market.
This new approach, which they called integrated lead discovery, was very complex and time-intensive. But, as Eder said, it was the only meaningful way forward for Factor D and also helped for Factor B.
In the end, after years of hard work, their approach yielded several valid compounds for both targets. This success was the fruit of a strong collaboration between chemists, structural biologists and biologists at different NIBR sites. “What really did the trick in our case was the fact that we had a great collaborative spirit on both sides of the Atlantic,” Flohr said. “Our collaboration not only included virtual meetings. We were also able to meet in person. During the COVID-19 pandemic, we lost this exchange. But it was very important at the time. I believe it helped the project advance.”
A new indication
Equipped with these compounds, Eder found support from Dick Harrison, an expert in complement system biology, to identify new indications and build a fresh clinical strategy. They identified a rare blood disease and several rare kidney diseases where dysregulation of the complement system is also driving disease activity.
“While the shift in indications was a big change, I was still convinced that the science of the compounds was strong enough for such a move,” Eder said. “Also, even though our research venture was no longer a company priority at the time, we were allowed to continue to invest some of our time in the project.”
Other colleagues who worked on the project at this stage included Anna Schubart, who developed new types of assays to test the compound’s validity in the new setting, and Stefanie Flohr, who originally chemically optimized some of the compounds.
Anna Schubart’s team developed cell-based assays to show whether the compounds would work against new disease indications.
Thanks to a hematology specialist, the team was able to access patient samples.
Flohr, a medicinal chemist, admits that when she joined the team she was a bit overwhelmed by the complexity of the underlying biology. But thanks to Anna Schubart, she came to terms with the complement system relatively quickly and both set out to further substantiate the new clinical strategy by internal work and through a network of external academic collaborations.
Patient cells
Schubart’s key focus was on developing new assays with which she could showcase the compound’s activity in the new disease indications. “My lab spent quite a long time setting up an in vitro assay to mimic the rare blood disease. And we were able to show that the compound was very potent in blocking the trigger of our disease,” Schubart said.
However, she lacked a key ingredient. “Despite our robust assays, we were not able to really convince the organization,” she said. “Assays may show strong results, but to prove that the compound works and to convince people to really move on, you need patient samples. That’s the holy grail.”


Stefanie Flohr
An atomic view of medicine.
Receiving the right patient samples is far from easy, especially in a rare indication, even for a leading player such as Novartis. But the team was lucky enough to find a sponsor in Antonio Risitano, a leader in hematology, who specialized in rare blood diseases, which the team had been focusing on.
Not only was he willing to test compounds using his patient samples, but he was also ready to collaborate on and lead the clinical trials once he saw the overwhelming positive results. “This really made all the difference,” Schubart said. “With the support from this clinical leader, we found a strong advocate for our case.”



Flohr’s lab helped turn the molecular lead into a compound ready for clinical development.
Strong science and human support
But while Risitano’s involvement was important, the pull from the Global Drug Development Team was crucial. “While we had produced convincing data, this in itself would not have been enough to push the project from discovery to development,” said Anna Schubart. “The fact that our colleagues from Global Drug Development were interested in our compound really moved things on and we were able to collaborate very closely with them.”
The Global Drug Development organization of Novartis, which includes more than 21 000 associates who are working on clinical trials, showed interest in the compound, as the organization was looking for new treatments that could help patients with rare blood diseases and other indications.
The fact that the chemical compound inhibited the complement system, which plays a role in several other diseases, was considered a great advantage to broaden the compound’s reach in other indications as well. The fact that the small-molecule drug would be administered orally was also considered a plus from a drug administration point of view.
The results of the ensuing experiments were overwhelmingly positive – propelling the project forward to the development team.
Although questions remained over the dosage and potential side effects of the compound, the project made quick progress once leaders such as Marty Lefkowitz and Thomas Holbro from Global Drug Development got involved in the process, adding increased speed and resources to the project, which together with NIBR was expedited to be tested in early trials and is now in late-stage clinical trial testing in several new indications.
“When I started as an observer on the project, it flew under the radar, so to speak,” Anna Schubart remembered. “If there hadn’t been the pull from the development organization, we would not have come so far. In essence, this means you really need people who believe in the science and who push you to the next level,” Schubart and Flohr agreed.



The team honed their focus on a rare blood disease, where they believed their approach had the greatest potential for success.
However, one key ingredient was missing: To gather convincing evidence, the team needed access to patient samples.
Sophie Sarret in the lab with Anna Schubart.
Also, for Joerg Eder, it was this combination of research expertise and human support that made all the difference. “Looking back from today’s vantage point,” Eder said, “all I can say is that what makes Novartis great came together in this project: the willingness to follow the science, the wish to collaborate across various functions and the readiness to test something new and take risks – and, of course, to help patients in need with the best possible science.”